Part 1: Why Focus on Kids?
As the year 2000 begins, the link between pesticides
and children has become a high profile issue for
consumer groups, the chemical manufacturing industry,
and government agencies. Even Congress is
getting into the act. "Pesticide risk unknown at schools" reads the headline of an Associated Press
article published in the January 5 Seattle Times. Senator Lieberman from Connecticut, Senator Torricelli from New Jersey, and our own Senator Murray are proposing new legislation that would require schools to notify parents before pesticides are used. Their concerns have been spurred by a recent General Accounting Office report which concluded that little is known about pesticide use in schools and the potential exposure of children.
Once again we find ourselves confronted with controversy and uncertainty about the health risks of pesticides. We have stepped into what has recently been called the "risk information vacuum" by two Canadian academics, Douglas Powell and William Leiss, in their
book, Mad Cows and Mother's Milk: The Perils of
Poor Risk Communication (McGill-Queen's University Press, 1997). It is always refreshing to view U.S. risk controversies through the eyes of our northern neighbors. Powell and Leiss sit outside the fray, and are
able to take a more sanguine look at the heated
health risk debates that seem to thrive in this country.
If we imagine the risk information vacuum from a chemist's perspective, we might see three sealed glass vessels in a line connected by stopcocks. The central vessel is a vacuum; one of its neighboring vessels contains various types of scientific knowledge; its other neighbor contains a mix of anecdotal information, speculation, anxiety, and even dread- let's call it "caution." If the two stopcocks are opened simultaneously, some combination of knowledge and caution will fill the vacuum. With pesticides and children we have a low concentration of scientific knowledge, but plenty of caution, so the vacuum quickly fills with a lopsided mixture. Until more scientific knowledge can be developed to supplant caution, the controversy continues.
Problems with Fleas
My own concern about children and pesticides was sparked by a series of informal side meetings held at national conferences of the American Chemical Society, starting about 1986. At the time I was at the Agricultural Experiment Station at Rutgers University in New Jersey, and my work dealt with fluorescent tracer evaluation of exposures during pesticide applications. In these meetings scientists from government, industry, and academia got together to discuss what we came to call the " indoor occupant exposure" issue. Our attention focused quickly on the use of indoor broadcast spraying and " bombs" (total release aerosol canisters) to control fleas. Several organophosphates and carbamates with moderate
acute toxicity were registered for this use. Scientists
at North Carolina State University (Wright, Leidy, and
others) had done some controlled spraying in dormitories,
and measured residues of such compounds as
chlorpyrifos and diazinon. Scientists at Dow had also
conducted a study of broadcast spraying of
Dursbanª. But none of these studies had systematically
estimated risks to children. What kinds of risks
did these treatments pose, we wondered?
Scientists from one major chemical manufacturer had
done some controlled spraying with their product, and
concluded that the possible risk for a crawling infant
in a home soon after broadcast treatment exceeded
their comfort zone. The company voluntarily withdrew
its product registration for broadcast application
around 1987.
I had done several research projects with scientists at Health Canada in Ottawa, and we soon found a common interest in this " new" issue of children's residential pesticide exposure. I was asked to develop exposure assessment guidelines for indoor environments, and in 1988 we tested the guidelines in a study with Dursban, following label instructions for broadcast treatment, and using some middle-of-the-road assumptions regarding skin contact and absorption. We published our findings in 1990 in the American Journal of Public Health (vol. 80, pp. 689-693), concluding that exposure levels within the first twenty-four to forty-eight hours "could result in doses at or above the threshold of toxicological response." Our findings were quite similar to those of the aforementioned industry scientists who had withdrawn their product for broadcast use. Seven years later Dow and United States Environmental Protection Agency (USEPA) agreed to remove broadcast and total release aerosol applications from the Dursban product label on
the basis of potential risks to children.
Children's Environmental Health
TABLE 1 CDC Action Levels for Blood Lead in Children |
|
Years |
Blood Lead Level (µg/dL) |
1960-1970 |
60 |
1970-1985 |
30 |
1985-1991 |
25 |
1991- |
10 |
If we have eliminated some of the high exposure scenarios for children and pesticides, why do concerns continue? Are children really at risk in schools? Do crack-and-crevice or lawn applications pose a hazard? To answer these questions we need to step away from the issue of pesticide safety and look more broadly at concerns about children's health. In the early 1990s a national network of public health professionals formed to focus on environmental hazards and children. The primary concern of this group was that children were being overlooked in research and health risk assessments. One result of their efforts was a 1996 Executive Order directing all federal agencies to develop an explicit strategy for including children's health in their evaluations. Now, researchers who apply for funding from the National Institutes of Health need to explain why they are not including children in their projects. The spotlight has clearly been shifted to reach children. Environmental health research now includes such questions as: what do children eat and how does it differ from adult diets? Where do children spend their time and how do they interact with their environment? How does hand-to-mouth activity in infants and toddlers affect exposure to environmental contaminants? Results from this research will add new knowledge to our understanding of pesticide health risks and reduce the uncertainty that currently fills the risk information vacuum. The National Institute for Environmental Health Sciences and the USEPA recently partnered in funding eight new "pediatric environmental health" research centers, one of which is here in the University of Washington's Department of Environmental Health. These new centers are part of the national effort to understand health risks in children.
Children and Susceptibility
The final element of concern related to children's health is children's susceptibility to certain environmental hazards. The discovery over the past two decades of the health effects of lead on children has been instructive. Since 1960 our estimate of an acceptable lead exposure level for children has decreased steadily, dropping from 60 to 10 micrograms per deciliter of blood, according to the Centers for Disease Control and Prevention (Table 1). Some scientists believe that effects can occur from exposures below 10 mg/dL; work is underway to test this hypothesis.
The lesson to be learned from lead exposure is that
children may have very different susceptibilities than
adults, particularly in the very early years of life. It is
well known, for instance, that infants have very low
levels of the enzyme methemoglobin reductase, making them particularly susceptible to anemia, or "blue baby syndrome." (See related article in AENews Issue 150,
Oct. 1998.) Also, the enzyme that breaks down the
pesticide parathion and its oxon derivative is not fully
expressed until about two years, so until that time young
children are probably at elevated risk from exposure.
These examples point to a need for a better understanding
of developmental factors in young children. Public
health is about the prevention of disease, and it is only
with a solid scientific base that we can develop policies
that are protective, fair, and cost-effective. Part 2 will
review our recent work on pesticide exposure in children
in Wenatchee.
Part 2: Children in Agricultural Communities
New concerns about pesticide health risks and children
in the late 1980s were the foundation for the
1996 Food Quality Protection Act. Those concerns
also spawned new efforts among public health scientists.
We saw the need for a better understanding of
exposure if we were to produce more accurate estimates
of risk. Equally important, we needed to
identify special populations at high risk.
Risk is often defined as the probability of harm. Groups at increased risk are normally those who either have high exposures or enhanced susceptibility to a particular disease agent. In the case of pesticides, for example, mixers, loaders, and applicators are considered "high risk" because of the relatively high exposure that can result from direct contact with commercial products and spray. Children are considered "high risk" because of possible increased susceptibility and the ongoing development of their organ systems.
So what about children of pesticide handlers and others who work with agricultural chemicals? Aren't their risks potentially high both from the point of view of exposure and of susceptibility? Our studies here at the University of Washington School of Public Health and Community Medicine for the past eight years have tried to answer these questions. We decided that children in farming communities should be defined as a special population for research, and that we needed to find out if their exposures and risks were different from those of other children. Furthermore, we knew that children in farming communities were probably exposed to more than one pesticide, and that pesticides that work by a common mechanism of action may produce an additive or cumulative risk. In the end we decided to focus our efforts on younger children (1-6 years old), and we examined their exposure to the organophosphorus (OP) insecticides.
Nearly all OP pesticides have a similar mode
of action: they inhibit the nervous system enzyme acetylcholinesterase.
Finding the Children
A major challenge for population-based exposure
assessment studies is defining the study population.
Sometimes this is done geographically or on the basis
of existing databases such as census data. Ideally, a
probabilistic sample can be drawn from a well-defined
population so that results can be generalized to the
larger population.
Defining "agricultural communities," however, turned out to be complicated. Such communities are widely dispersed and do not always conform to census or political boundaries.
Once the community is defined, traditional methods of access to families may not be feasible. Among agricultural workers, multiple families may live in residences designed for a single family, and telephone- based sampling methods may miss a significant fraction of the population. In our state's agricultural regions the primary language of many workers is Spanish, so bilingual capabilities are essential.
The area selected for our studies centered around
Wenatchee, Washington. The region consists of an urban zone along the Columbia River, with orchards extending into the surrounding mountain canyons as well as upriver, and newer residential development interspersed with farmland. This entire region was considered the "agricultural community" for our studies. Orchard management in the area includes periodic application of several OP pesticides, including azinphos-methyl, chlorpyrifos, diazinon, phosmet,
and malathion.
In our recent studies we attempted probability-based
sampling using census tract data, but this approach
required a randomized door-to-door contact, as much
of the population did not have telephone service. We
also found that families were wary of strangers approaching
their doors, and were often unreceptive to
our request for participation. This method was ultimately
abandoned as impractical. Study participants
were recruited through community organizations,
including social service agencies, clinics, and producer-
operated cooperatives. This approach allowed
us to quickly identify families with young children.
Our studies in 1992 and 1995 divided households into two groups based on proximity to farmland and parental occupation. " Agricultural" families were defined as households that included at least one adult working in farming. Adult workers were further classified as pesticide applicators and farm workers in the 1995 study. None of the pesticide applicators in these studies conducted this activity full-time. A smaller "reference" family population was also recruited. These families had no household members working in farming, and lived more than one-quarter of a mile (about 400 meters) from farmland. Children up to six years of age were recruited from these families. Often more than one child per family would participate in the study.
Assessing Exposures
 When we began this work in 1991 there were no
laboratories prepared to conduct multiple OP residue
analysis in media other than food. Even acquiring
appropriate standards was problematic. Our lab had
to develop new analytical
methods to meet our
needs for environmental
measurements. Our
1992 and 1995 studies
focused on four OP
pesticides used in
Washington state orchards:
azinphos-methyl,
phosmet, chlorpyrifos, and ethyl parathion. We included soil and house dust sampling.
When we began this work in 1991 there were no
laboratories prepared to conduct multiple OP residue
analysis in media other than food. Even acquiring
appropriate standards was problematic. Our lab had
to develop new analytical
methods to meet our
needs for environmental
measurements. Our
1992 and 1995 studies
focused on four OP
pesticides used in
Washington state orchards:
azinphos-methyl,
phosmet, chlorpyrifos, and ethyl parathion. We included soil and house dust sampling.
Thirty OP pesticides
were registered for use
in Washington State in
1998. Studies expanded
to include diazinon, dichlorvos, malathion,
methyl parathion, methidathion, mevinphos, ethoprop, phorate, dimethoate, and terbufos; sample media were expanded to include
twenty-four-hour indoor air, indoor and outdoor
surface wipes, and drinking water. Duplicate one-day
diet samples were analyzed by Dr. Carol Weisskopf at
the Food and Environmental Quality Laboratory at
Washington State University. Nonetheless, more than
half of the OP pesticides registered in Washington
State still fell outside these analytical capabilities.
Biological monitoring for multiple OP compounds is also challenging. Of the thirty pesticides used in Washington, for example, only five have compound specific urinary metabolites. The lack of specific metabolites for OP pesticides led us to measure urinary dialkylphosphates - the common metabolites
of the OPs. Six metabolic products are normally
measured by gas chromatography following derivatization: dimethyl phosphate (DMP), dimethylthio phosphate (DMTP), dimethyldithio
phosphate (DMDTP), diethyl phosphate (DEP), diethylthio phosphate (DETP), and diethyldithio
phosphate (DEDTP). It
is important to realize,
though, that even this
more generic assay
does not necessarily
capture all OP compounds.
Eight of the
thirty OP pesticides
used in Washington are
not measured with this
technique.
Pesticide
Levels in
Homes
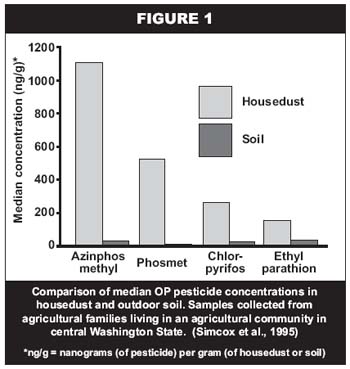
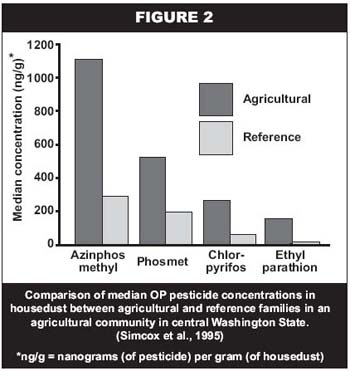 The 1992 studies included soil and house dust sampling of forty-eight agricultural families and eleven reference families. Figure 1 provides median values for four OP pesticides in house dust and soil. These data indicated that house dust concentrations were substantially higher than soil concentrations for all compounds, and that the highest house dust concentrations were for azinphos-methyl and phosmet, both dimethyl compounds. These findings, coupled with knowledge that these children spent much of their time indoors, led to the conclusion that house dust concentration was the most useful indicator of exposure potential for this population. Figure 2 compares the OP pesticide house dust concentrations for agricultural and reference families, demonstrating that children in agricultural households had higher exposure potential than did children in reference families for all four OP compounds measured.
The 1992 studies included soil and house dust sampling of forty-eight agricultural families and eleven reference families. Figure 1 provides median values for four OP pesticides in house dust and soil. These data indicated that house dust concentrations were substantially higher than soil concentrations for all compounds, and that the highest house dust concentrations were for azinphos-methyl and phosmet, both dimethyl compounds. These findings, coupled with knowledge that these children spent much of their time indoors, led to the conclusion that house dust concentration was the most useful indicator of exposure potential for this population. Figure 2 compares the OP pesticide house dust concentrations for agricultural and reference families, demonstrating that children in agricultural households had higher exposure potential than did children in reference families for all four OP compounds measured.
Our 1995 studies included house dust sampling in seventy-six homes and collection of urine samples from 109 children. An initial report of this study compared DMTP urinary concentrations of forty-eight applicator children and eleven reference children.
The patterns for metabolite concentrations were similar to those for house dust concentrations: about a four- to five-fold difference between the groups.
Our studies in 1998 included biweekly urine samples
from about fifty Wenatchee children for one year,
samples from 100 children in two Seattle metropolitan
area communities, and a pilot multi-pathway exposure
analysis in thirteen homes. We are hoping to publish
results for these studies sometime this year.
What Are the Risks?
Translating the environmental and biological measurements we have collected into a meaningful statement about health risk has not been a simple task. First, we felt that the parents of the children who participated in our studies deserved clear and understandable feedback about the study results. The letters we sent to parents included specific results for their children, but also tried to answer the question, "Should I be concerned about these levels from a health standpoint?" We told parents that the levels we measured did not pose a serious or immediate hazard to their children, and that exposures were best described as "low level." We became convinced after comparing our study results with available scientific information that these children were not at risk for an acute health effect, such as substantial decrease in their nervous system enzymes. Yet when it comes to more subtle health effects, we don't have a good answer. The jury is still out. A number of studies are exploring the effects of low-level OP pesticide exposure on neurological development in very young animals. New findings will be reported periodically in the scientific literature, and will perhaps even reach the newspapers. But it will be many years before the question of long-term effects will be answered with any reasonable degree of scientific certainty. In the meantime, what do we do?
Public health emphasizes prevention as the most effective means of reducing risk. We have encouraged parents who wish to reduce their children's exposure to adopt some commonsense procedures: always follow pesticide label instructions, keep pesticides in a safe place in the home, remove shoes and clothing that may have pesticide residues before entering the home, and keep kids away from pesticide-treated areas, both indoors and out. We have also joined with scientists at the Fred Hutchinson Cancer Research Center to develop a study in the lower Yakima Valley to see if a community- based education program can reduce pesticide exposure in children of agricultural workers.
The debate about pesticide health risks is likely to be a long and contentious one. The scientific uncertainty that has created the current risk information vacuum means that caution will be an important principle in regulation. In the meantime, good public health practice and common sense suggest we try to reduce our children's exposures wherever possible.
REFERENCE AND ADDITIONAL RESOURCES
Eskenazi B., Bradman A., Castorina R. Exposures of children
to organophosphate pesticides and their potential adverse
health effects. Environmental Health Perspectives
Supplements 1999: Vol. 107, pp. 409-419.
Loewenherz C., Fenske R.A., Simcox N.J., Bellamy G.,
Kalman D.A. Biological monitoring of organophosphorus
pesticide exposure among children of agricultural workers
in central Washington State. Environmental Health
Perspectives 1997, Vol. 105, pp. 1344-1353.
Simcox N.J., Fenske R.A., Wolz S.A., Lee I.C., Kalman D.A.
Pesticides in household dust and soil: exposure pathways
for children of agricultural families. Environmental Health
Perspectives 1995, Vol. 103, pp. 1126-1134.
Part 3: Estimating Doses for Children
In the February and March issues
of Agrichemical and Environmental
News (AENews Nos. 166 and 167), I shared some background on the concerns surrounding children's exposure to pesticides and I outlined University of Washington (UW) studies on children in the Wenatchee area. In the last
week of April, a new analysis of our
Wenatchee studies was published in Environmental Health Perspectives, a scientific journal sponsored by one of the National Institutes of Health (see Editor's Note, p. 3). Once published, a paper like this can become news, and this one did. The information released by the University of Washington Office of Health Sciences and Medical Affairs was headlined: "UW Study Finds Many Farm Children Are Exposed to Pesticides." This was translated in the Seattle Times on April 25, 2000, as " Kids' Pesticide Levels Unsafe."
Why did our findings draw media attention? Did our paper really demonstrate that children are exposed to pesticides at "unsafe" levels?
In our report, we tried to answer the question that parents and others ask when they learn about our studies of children and pesticides: "What are the risks? Are the levels safe?" These are not easy questions to answer.
Methodology in Brief
Our study evaluated the exposures of 109 children living in Chelan and Douglas counties. Most (91) had parents working in agriculture. The others (18) did not have any household members involved in agriculture, and lived at least one-quarter mile from treated farmland. The metabolites we measured in the children's urine are common to several organophosphorus
(OP) pesticides,
including azinphos-methyl and
phosmet. Our approach was to
convert the OP pesticide metabolites
found in the urine of children
to estimates of the total amount of
pesticides the children probably
absorbed on the day we sampled.
These dose estimates were then
compared to guidelines developed
by the Environmental Protection
Agency and the World Health
Organization (Table 1). Our analysis
assumed that the metabolites
were the result of exposure to
either azinphos-methyl orphosmet, the two chemicals found in nearly all of the house dust samples we collected from the children's homes. The results are presented in Table 2, and a graph of dose distribution is presented as Figure 1.
TABLE 1 |
||
| Children's OP pesticide doses relative to the U.S. Environmental Protection Agency chronic dietary reference doses (RfDs), and World Health Organization acceptable daily intakes (ADIs) for azinphosmethyl and phosmet1 | ||
| Regulatory Reference Value | Agricultural Children |
Reference Children |
% of spray season dose estimates exceeding reference value2 |
||
| EPA Chronic Reference Dose (RfD) | ||
| Azinphos-methyl (1.5 µg/kg/d) | 56 |
44 |
| Phosmet (11 µg/kg/d) | 8.9 |
0 |
| WHO Acceptable Daily Intake (ADI) | ||
| Azinphos-methyl (5 µg/kg/d) | 19 |
22 |
| Phosmet (20 µg/kg/d) | 3.3 |
0 |
| 1 Includes all children in the study; assumes doses are attributable entirely to either azinphos-methyl or phosmet. 2 Based on 91 estimates for agricultural children and 18 estimates for reference children. |
||
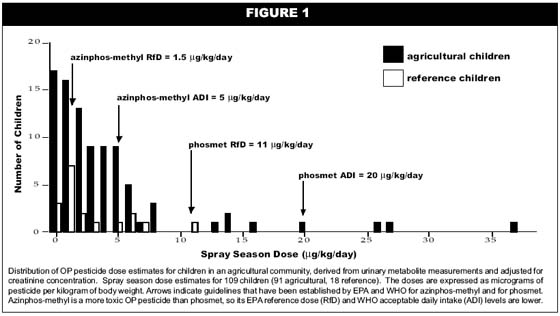
Findings in Brief
We found that for children whose parents worked in agriculture as either orchard applicators or field-workers, more than half of the doses estimated for the spray season exceeded the U.S. Environmental Protection Agency's chronic dietary reference dose (RfD) and about one fifth exceeded the World Health Organization's acceptable daily intake (ADI) values for azinphos-methyl. For children
whose parents did not work in agriculture
the values were 44% and 22%, respectively.
When we considered that the metabolites
were due to phosmet exposure, we found that less than 10% of the children exceeded the EPA and WHO reference values. None of the dose estimates exceeded what is called the "no effect" level determined in animal studies. We also noted that the study took place during a period of active spraying, and we cautioned readers not to generalize to other times of the year, or other
regions. Nevertheless, it seems reasonable to
assume that these children were exposed at these
levels across the 40 to 50 days of the spraying
season.
The Public Health Message
What do these numbers and comparisons really mean for children's health? The major public health message is that these findings are cause for concern, but not for alarm. We can say with some certainty that these exposures fall short of causing acute health effects, since the WHO and EPA guidelines incorporate large uncertainty factors. But it is also clear that the exposures for many of these children fall into that zone of uncertainty.
TABLE 2 |
||||
| Spray season dose estimates1 adjusted by daily creatinine output. Children were aged 0-6 years. Doses were based on two dialkylphosphate metabolites (DMTP and DMDTP) common to the dimethyl organophosphorus pesticides. | ||||
Dose (µg/kg/day) |
||||
Applicator children (n=49) |
Farmworker children (n=13) |
Agricultural children2 (n=62) |
Reference children (n=14) |
|
| Median | 2.8 3,4 |
1.2 3 |
2.0 5 |
0.3 4,5 |
| 25th percentile | 0.8 |
0.6 |
0.7 |
0.1 |
| 75th percentile | 4.4 |
4.1 |
4.3 |
3.2 |
| Mean | 3.8 |
2.4 |
3.5 |
2 |
| Std. Dev. | 4.6 |
2.5 |
4.2 |
3.1 |
| Range | 0 - 19.5 |
0 - 7.5 |
0 - 19.5 |
0 - 10.3 |
| 1 Spray season dose estimates were based on the average of two samples per child. Only one child was used from each family in this analysis. All samples were collected during the May-July spraying season. In cases with missing samples, a single sample was used to estimate average dose. 2 Agricultural children are a combination of applicator and farmworker children. 3 Applicator and farmworker children dose estimates were not statistically different (Mann-Whitney U Test). 4 Applicator and reference children dose estimates were statistically different (p=0.05, Mann-Whitney U Test). 5 Agricultural and reference children dose estimates were marginally different (p=0.06). |
||||
Some will argue that the current guidelines are too
stringent, but others argue that they are not protective
enough, particularly for children. Current regulatory
methods are based on measurements of residues in
food, water, and the environment, from which models
are developed to estimate dose. Often these models
include very conservative or protective assumptions,
which can lead to high estimates and the appearance
of risk that may or may not be present. Biological
monitoring data are not normally used in the regulatory
process, as they are very cumbersome to obtain
and complex to coordinate. Yet it seems clear that
they can provide a more accurate estimate of the
dose that a child receives. The primary scientific
message is that biological measurements, such as
pesticide metabolites in urine, can give us reasonably
good estimates of dose and risk. As we monitor more
children we will be able to see patterns that can aid in
developing commonsense and cost-effective methods
to reduce exposures.
Dr. Richard Fenske is Professor of Environmental Health at the University of Washington's School of Public Health and Community Medicine, and Director of the Pacific Northwest Agricultural Safety and Health Center (PNASH). He also serves on EPA's Science Review Board, a congressionally mandated advisory board for pesticide science policy. He can be reached at rfenske@u.washington.edu or (206) 616-1958.
Disclaimer and Reproduction Information: Information in NASD does not represent NIOSH policy. Information included in NASD appears by permission of the author and/or copyright holder. More