SUMMARY
In the summer of 2013, a male general laborer in his 60s died due to hypertensive and arteriosclerotic cardiovascular disease while working outdoors on a hot day. The decedent was conducting grounds keeping work at a machinery moving, warehousing and transportation facility. He worked for several hours in the morning cutting tree limbs. When enough of the cut limbs had been accumulated, he used a backhoe to move the limbs to another area of the facility. At approximately 10:00 a.m., a coworker noticed that the backhoe was stationary where the limb storage area was located. The employee investigated and found the decedent non-responsive and slumped forward in the seat of a non-air conditioned cabbed backhoe. CPR was initiated by employees while emergency response was called. Emergency responders assumed care upon arrival and transported him to a local hospital where he was pronounced dead.
Factors contributing to the death:
RECOMMENDATIONS
During the summer of 2013, a male laborer in his 60s died due to medical issues complicated by hyperthermia. MIFACE learned of this incident from MIOSHA. MIFACE contacted the safety director of decedent’s employer who agreed to participate with the MIFACE program. During the writing of this report, the police department report, autopsy, and death certificate were reviewed.
The decedent’s employer had been in business for more than 50 years. They specialized in machinery moving, warehousing and transportation. The decedent was a seasonal part-time employee. He provided general labor for the firm, such as truck driving, grounds keeping, and any other work he was asked to do. The decedent worked 8-hour days while at the firm. He worked at the firm while in Michigan and then wintered in another state. He had been employed by the firm in this capacity for two years.
The firm had a written health and safety program and provided safety and health training. The program did not have a specific section relating to heat illness prevention. During the summer months, the firm provided employees Gatorade and other cold beverages free of charge, which could be transported to the employee work site in their lunch coolers. The firm had a joint management/labor safety committee that met at least quarterly or more frequently if a specific issue arose. The firm had not conducted heat stress training to its employees.
MIOSHA determined this death to be a non-program-related death based on the preliminary information reported and did not conduct an investigation.
The decedent had previously owned a gravel hauling business, from which he had retired. The safety director indicated the decedent had operated backhoes and other heavy equipment for many years.
The backhoe involved in the incident had a cab and was not air-conditioned. It is unknown if the cab doors were open when occupied. The safety director could not recall the name of the backhoe manufacturer. MIFACE did not have an opportunity to look at the backhoe.
The decedent arrived at the facility at approximately 7:00 a.m. He did not indicate to his coworkers prior to starting his work that he was feeling ill, etc. He began cutting tree limbs with a chain saw and performed other grounds keeping duties. When enough branches had been trimmed, he used the backhoe to transport the branches to another area of the property. The decedent was last seen by fellow employees at approximately 9:00 a.m.
The event was unwitnessed.
At approximately 10:00 a.m., a coworker saw the backhoe stationary in the location where the decedent was placing the trimmed branches. This employee went to investigate and found the decedent sitting on the seat motionless, slumped over and unresponsive. The employee called 911 and notified the safety director. His coworkers removed him from the backhoe and laid him on the ground. They performed CPR until emergency response arrived and assumed care. He was transported to a local hospital where he was pronounced dead.
The hospital record indicated the decedent’s current medications were Aleve®; Motrin®; a beta-adrenergic blocking agent, which can be used for high blood pressure, heart pain, abnormal rhythms of the heart and neurologic conditions; and a cholesterol lowering agent. The hospital record and the medical examiner report did not state that a core body temperature was taken to confirm the diagnosis of hyperthermia.
Weather data was obtained from Weather Underground (www.weatherunderground.com) for the incident location, for three days prior to the incident and on the incident day. Table 1 shows the temperature, dew point, relative humidity, wind speed, conditions (clear, cloudy, etc) and calculated heat index (as performed by Weather Underground). Humidity the amount of water vapor within a given space is commonly measured as the relative humidity (RH), i.e., the percentage of moisture in the air relative to the amount it could hold if saturated at the same temperature. High dew point numbers (55°F to 75°F+) indicates that it feels "sticky" outside. Dew point values of 30°F or lower show indicate it feels “dry” outside.
The incident day was clear. When he arrived at work at 7:00am, he had a clear day (sunny). The temperature was 730F with a relative humidity of 90%. By 9:00am, the temperature had risen to 800F but the relative humidity had decreased to 79%.
The cause of death as listed on the death certificate was Hypertensive and Arteriosclerotic cardiovascular disease. The manner of death was accidental. The medical examiner’s autopsy report indicated that hyperthermia was a significant condition contributing to his death. The medical examiner described how the injury occurred as “Exposure to Hot Environment.” However, neither the admitting hospital or the medical examiner did not measure the core body temperature at time of death. Toxicology tests noted caffeine only.
| Three Days Prior to Incident | Two Days Prior to Incident | One Day Prior to Incident | Day of Incident | |
| Temperature (°F) | 8:00am: 75.1 | 8:00am: 77.0 | 8:00am: 77.0 | 8:00am: 75.9 |
| 9:00am: 80.1 | 9:00am: 80.1 | 9:00am: 81.0 | 9:00am: 80.1 | |
| 10:00am: 84.0 | 10:00am: 82.0 | 10:00am: 84.9 | 10:00am: 84.0 | |
| Dew Point (°F) | 8:00am: 71.1 | 8:00am: 73.9 | 8:00am: 72.0 | 8:00am: 72.0 |
| 9:00am: 72.0 | 9:00am: 73.9 | 9:00am: 73.0 | 9:00am: 73.0 | |
| 10:00am: 73.0 | 10:00am: 73.9 | 10:00am: 75.0 | 10:00am: 73.9 | |
| Humidity (%) | 8:00am: 85 | 8:00am: 90 | 8:00am: 84 | 8:00am: 87 |
| 9:00am: 76 | 9:00am: 81 | 9:00am: 77 | 9:00am: 79 | |
| 10:00am: 69 | 10:00am:76 | 10:00am: 72 | 10:00am: 72 | |
| Wind (mph) | 8:00am: Calm | 8:00am: 3.5 | 8:00am: 3.5 | 8:00am: 4.6 |
| 9:00am: Calm | 9:00am: 4.6 | 9:00am: 4.6 | 9:00am: 4.6 | |
| 10:00am: Calm | 10:00am: 5.8 | 10:00am: 5.8 | 10:00am: 3.5 | |
| Conditions | 8:00am: Clear | 8:00am: Clear | 8:00am: Clear | 8:00am: Clear |
| 9:00am: Clear | 9:00am: Clear | 9:00am: Clear | 9:00am: Clear | |
| 10:00am: Scattered Clouds | 10:00am: Mostly Cloudy | 10:00am: Clear | 10:00am: Clear | |
| Calculated Heat Index (°F) | 8:00am: -- | 8:00am: -- | 8:00am: -- | 8:00am: -- |
| 9:00am: 83.8 | 9:00am: 84.5 | 9:00am: 85.8 | 9:00am: 84.2 | |
| 10:00am: 90.2 | 10:00am: 87.9 | 10:00am: 93.9 | 10:00am: 91.2 |
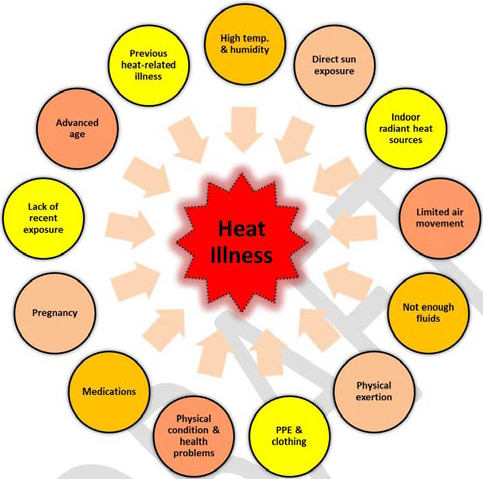
Figure 4.1. Examples of some of the risk factors of heat-related
illness. Courtesy of NIOSH Draft Document: Criteria for a
Recommended Standard – Occupational Exposure to Heat
and Hot Environments
*Michigan-specific information at the MIOSHA website A to Z Topic Index; a topic devoted to Heat Stress is available. Additional Heat Stress presentations developed by MIOSHA staff are available when “heat stress” is entered in the Search box on the MIOSHA website.
*NIOSH has a topic page on its website dedicated to heat stress resources at http://www.cdc.gov/niosh/topics/heatstress/ . Included on the topic page are types of heat stress, recommendations for employers and workers, additional resources from other government agencies, NIOSH Fast Facts: Protecting Yourself from Heat Stress (available in English and Spanish), and NIOSH publications including Criteria for a Recommended Standard . . . Occupational Exposure to Hot Environments. Revised Criteria 1986. The documents are also available by calling 1-800-356-4674.
*OSHA has additional heat stress resources as part of their heat illness national campaign available at https://www.osha.gov/heat/index.html
* NIOSH is in the process of updating the Criteria Document on hot environments to reflect recent research and findings. The Draft Document: Criteria for a Recommended Standard: Occupational Exposure to Heat and Hot Environments can be found here. All recommendations in this report are drawn from this draft document.
Employers should establish a heat illness prevention program to ensure employee health and safety while working in locations where elevated temperatures and humidity exist. The intent of the program should be to ensure that an individual’s core body temperature is maintained as close to normal as possible.
The company did not have a heat illness program nor did they provide training on heat stress. The decedent’s employer recognized the potential health hazards of heat by supplying free Gatorade and other cold beverages to the employees. It is unknown if the other beverages contained caffeine. The employer had no medical program to ensure that employees were fit to work in hot environments.
A heat illness program utilizes (at a minimum) employee training and acclimatization, engineering and work practice controls, medical surveillance, and recordkeeping to protect workers from the adverse health effects caused by excessive heat exposure. In this incident, a heat illness prevention program would have reduced the likelihood of the occurrence of this individual’s death.
A heat stress training program should be developed and implemented when individuals will work in hot and/or humid environments. These individuals should receive training about the prevention of heat-related illness before beginning work in a hot environment and/or before heat index levels rise. Training should be reinforced on hot days. Prevention of serious heat-related illnesses is dependent on early recognition of the signs and symptoms of impending heat-related illness and initiation of first aid and/or corrective procedures at the earliest possible moment.
Part of the training program should be to inform employees to identify if they are at higher risk. Employers may also want to consider medical fitness exams with a healthcare provider familiar with the health effects of heat to advise regarding the need for medical restrictions. See below.
When working outside, heat stress controls utilizing work and hygienic practices are the most practical (compared to engineering controls) to prevent heat illness. A written Heat-Alert Program should be developed and implemented whenever the National Weather Service or other competent weather forecast service forecasts that a heat wave is likely to occur the following day or days. A heat wave is indicated when daily maximum temperature exceeds 350C (950F) or when the daily maximum temperature exceeds 320C (900F) and is 50C (90F) or more above the maximum reached on the preceding days.
A medical surveillance program is recommended because although all workers are at risk of heat stroke, workers with certain medical conditions and/or taking certain medications are at an increased risk. The medical assessment should be conducted by a health care provider familiar with the health effects of heat. The assessment should be performed include pre-placement medical examinations for those persons who are candidates for a job in a hot environment and periodic medical examinations for those workers who are work in such jobs.
Medications that can place a person at increased risk if exposed to heat and/or humid environments include:
| Anticholinergics | Impaired sweating |
| Antihistamines | Impaired sweating |
| Phenothiazines (Thorazine®, Stelazine®, Trilafon®) | Impaired sweating, (possibly) disturbed hypothalamic temperature regulation |
| Tricyclic antidepressants (imipramine, amitriptyline) | Impaired sweating, increased motor activity and heat production |
| Amphetamines, cocaine, “Ecstasy” | Increased psychomotor activity, activated vascular endothelium |
| Ergogenic stimulants (ephedrine/ephedra) | Increased heat production |
| Lithium | Nephrogenic diabetes insipidus and water loss |
| Diuretics | Salt depletion and dehydration |
| Antihypertensives (atenolol, carvedilol) | Reduced skin blood flow and reduced blood pressure |
| Ethanol | Diuresis, possible effects on intestinal permeability |
| Barbiturates | Reduced blood pressure |
| Antispasmodics | Impaired sweating |
| Haloperidol | Tachycardia, altered central temperature regulation, and hyponatremia |
Medical conditions that can increase an individual’s risk of a heat-related illness are: history of myocardial infarction; congestive heart failure; coronary artery disease; severe obstructive or restrictive pulmonary disease; diabetes; a history of skin disease covering large percent of the body; an injury to a large area of the skin; an impairment of the sweating mechanism that might impair heat elimination via sweat evaporation from the skin; gender and obesity.
No condition was identified on his autopsy that placed the decedent at increased risk of mortality from heat. The decedent was a non obese male in his mid-60s. On autopsy, the decedent was noted to have caffeine in his blood. He used medications to control blood pressure and cholesterol, although not the medications listed above. Recent studies suggest that caffeine may have less effect on heat tolerance than previously suspected. Caffeine is a mild diuretic and may reduce fluid volume resulting in cardiovascular strain during exposure to the heat. Water is considered the most optimal, hydrating beverage for a worker to drink before, during, and after work. It is suggested to match fluid loss from the body with fluid intake. This requires drinking about 150 to 200 mL (5 to 7 ounces) every 15 to 20 minutes.
Recordkeeping is important to document employer and employee information as related to heat illness incidents and prevention activities. Recordkeeping can include measurements of environmental heat exposure, medical surveillance records, report of heat illness and environment and work conditions at the time of the incident, and heat acclimatization procedures.
Employers should obtain local climate data to identify periods of high heat and/or high dew points and humidity in order to adjust the work duties for the conditions of the day, schedule adequate water and rest breaks, and maintain watchfulness for signs of heat illness in the workers. Tools such as the heat index are available to assist the employer in assessing environmental conditions.
When individuals work in environments with a high humidity, sweating continues (increasing the level of dehydration), but the evaporation of sweat is inhibited, heat transfer from the body is reduced and the internal body temperature increases. Thus, when the heat index is greater than 95°F and is largely due to high humidity, the evaporative heat loss is virtually nonexistent. Consequently, even if the ambient dry temperature is within a comfortable range (e.g., 73°F), the high humidity could result in an “apparent temperature” or heat index high enough to create heat stress to the worker that is great enough to present the possibility of heat illness or injury [Taylor et al. 2008].
When discussing heat illness, the local microclimate is important – what surface, presence/absence of wind, presence/absence of shade, clothing worn, etc. may create a microclimate much hotter than the general outdoor temperature.
Table 2 (below) is copied from the Using the Heat Index: A Guide for Employers referenced in the paragraph above. Table 2 presents an approach for setting work/rest schedules for workers wearing normal clothing drawn from the US EPA/OSHA joint publication, A Guide to Heat Stress in Agriculture. Table 2 used an adjusted temperature calculation to approximate the Wet Bulb Globe Temperature (WBGT). Table 1 may be used when instruments which measure WBGT are unavailable and when there is perceptible air movement. While Table 2 allows 13° for the full heating effect of the sun, the effect of solar heat can be greater under some conditions. Where there is little or no air movement, Table 2 is not appropriate.
| Adjusted Temperature* Calculated | Light Work | Moderate Work | Heavy Work |
|---|---|---|---|
| 90 | Normal | Normal | Normal |
| 91 | Normal | Normal | Normal |
| 92 | Normal | Normal | Normal |
| 93 | Normal | Normal | Normal |
| 94 | Normal | Normal | Normal |
| 95 | Normal | Normal | Normal |
| 96 | Normal | Normal | Normal |
| 97 | Normal | Normal | Normal |
| 98 | Normal | Normal | Normal |
| 99 | Normal | Normal | Normal |
| 100 | Normal | 45/152 | 30/30 |
| 101 | Normal | 40/20 | 30/30 |
| 102 | Normal | 35/25 | 25/35 |
| 103 | Normal | 30/30 | 20/40 |
| 104 | Normal | 30/30 | 20/40 |
| 105 | Normal | 25/35 | 15/45 |
| 106 | 45/152 | 20/40 | Caution3 |
| 107 | 40/20 | 15/45 | Caution3 |
| 108 | 35/25 | Caution3 | Caution3 |
| 109 | 30/30 | Caution3 | Caution3 |
| 110 | 15/45 | Caution3 | Caution3 |
| 111 | Caution3 | Caution3 | Caution3 |
| 112 | Caution3 | Caution3 | Caution3 |
| Note: Adjust the temperature reading as follows before going to the temperature column in the table: | |||
| Full Sun (no clouds) | Add 13° | ||
| Partly cloudy/overcast | Add 7° | ||
| No shadows visible/work is in the shade or at night | No adjustment | ||
| For relative humidity of: | |||
| 10% | Subtract 8° | ||
| 20% | Subtract 4° | ||
| 30% | No adjustment | ||
| 40% | add 3° | ||
| 50% | add 6° | ||
| 60% | add 9° | ||
| For example, if the temperature is 91°, it is dusk the relative humidity is 40%, and heavy work is to be done, such as moving heavy materials with a wheelbarrow: | Start with 91° and add 3° because the humidity is 40% [91°+3°=94°]. Go to 94° in the table; under these conditions, it would be reasonable to follow a normal work schedule. | ||
NOTES:
On the day of the incident, Table 1 shows that although the humidity was declining, the temperature was rising. It was a sunny day. At 9:00 a.m., the temperature was 80°F and the humidity was 79%. Using the guidelines shown in Table 2:
*Day was sunny – add 13°F: 80 + 13= 93°F.
*Day was humid – greater than 60% - add 9°F: 93 + 9 = 102°F
The assumptions used in the table include physically fit, fully hydrated heat-acclimatized adults under the age of 40 years. The decedent was over 60 years of age. At a minimum, the work recommendations calculated for the decedent indicate that he should have been working 20 minutes with rest periods of 40 minutes, or better yet, not at all under these conditions due to the likelihood that, with the sun shining, the non-air-conditioned backhoe was most likely hotter than the outdoor temperature. This individual was exposed to dangerous levels of environmental heat stress.
To protect employees from heat illness, it may be necessary to schedule heavy work activities during cooler periods, such as morning or evening, or to shorten working periods and increase rest periods to ensure workers have an appropriate recovery period from the heat. Rest breaks provide time to drink water and allow the body to cool down. Breaks should be taken in cool, shady areas, possibly even air conditioning. Workers should drink water every 15 minutes, even if not thirsty. For specific guidelines on setting work and rest schedules, see the OSHA Heat Illness topic page; Using the Heat Index: A Guide for Employers: https://www.osha.gov/SLTC/heatillness/heat_index/pdfs/work_rest_schedules.pdf.
Another tool to calculate the heat index for a work site is the use of a smart phone application, such as OSHA’s Heat Safety Tool (www.osha.gov/SLTC/heatillness/heat_index/heat_app.html). The App allows workers and supervisors to calculate the heat index for their worksite, and, based on the heat index, displays a risk level to outdoor workers. Then, with a simple “click,” one can get reminders about the protective measures that should be taken at that risk level to protect workers from heat-related illness-reminders about drinking enough fluids, scheduling rest breaks, planning for and knowing what to do in an emergency, adjusting work operations, gradually building up the workload for new workers, training on heat illness signs and symptoms, and monitoring each other for signs and symptoms of heat-related illness.
Acclimatization is the body’s improved response to heat stress after exposure to environmental heat and strenuous physical exertion. It allows the body time to adjust to working in hotter temperatures by improving the sweating mechanism and allowing the body to better maintain appropriate body temperature and heart rates. According to NIOSH, it takes approximately five 12 to seven days for an individual to acclimatize to a hot environment. Employers should manage employee work load to include assigning lighter duties, providing longer rest periods, gradually increasing the level of work each day, and monitoring how the workers respond to working in the heat. It is important that workers complete the full acclimatization period. Even after acclimatization, workers still may not work as effectively in high heat and humidity. Employers and employees should recognize that an acclimatized person begins losing acclimatization within four days.
Acclimatization does not reduce the need for water or rest breaks. Acclimatized workers still require adjusted work/rest schedules during periods of high heat and humidity. Work/rest schedules set for acclimatized workers should not be used as an acclimatization schedule for the non-acclimatized worker.
The acclimatization period should be tailored to local conditions, type of clothing worn, type of work, and the worker. An acclimatization program should be implemented for the following:
Interestingly, the largest number of heat-related deaths related occur in May, when temperatures have just risen, rather than in July or August. This is similar to the ‘rapid change’ category. Employers should alert employers to the specific risks of warmer spring weather.
MIFACE (Michigan Fatality Assessment and Control Evaluation), Michigan State University (MSU) Occupational & Environmental Medicine, 909 Fee Road, 117 West Fee Hall, East Lansing, Michigan 48824-1315; http://www.oem.msu.edu. This information is for educational purposes only. This MIFACE report becomes public property upon publication and may be printed verbatim with credit to MSU. Reprinting cannot be used to endorse or advertise a commercial product or company. All rights reserved. MSU is an affirmative-action, equal opportunity employer.
Publication #: #13MI090 | June 25, 2014
Disclaimer and Reproduction Information: Information in NASD does not represent NIOSH policy. Information included in NASD appears by permission of the author and/or copyright holder. More